Addison's disease is an endocrine or hormonal disorder.
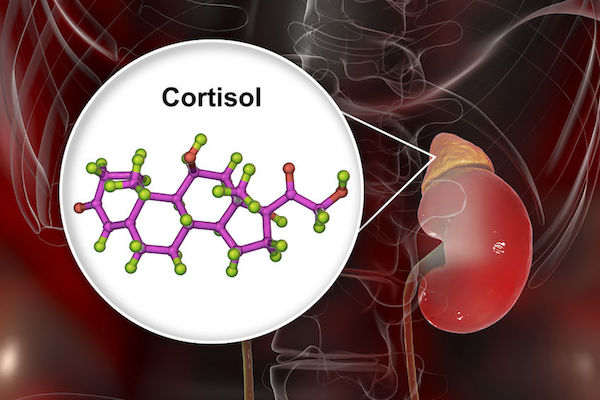
Addison's disease occurs when the adrenal glands fail to produce enough of the hormone cortisol and, in some cases, the hormone aldosterone. The adrenal glands are two small glands that sit on top of the kidneys. They produce two essential hormones: cortisol and aldosterone.
In Addison's disease, the adrenal gland is damaged, and not enough cortisol and aldosterone are produced.
The condition is usually the result of a problem with the immune system, which causes it to attack the outer layer of the adrenal gland (the adrenal cortex), disrupting the production of steroid hormones aldosterone and cortisol.
Tuberculosis (TB), an infection that destroys the adrenal glands, reportedly accounts for about 10 to 15 percent of cases of primary adrenal insufficiency in developed countries.
Rarely is Addison’s disease hereditary.
What are its symptoms?
Addison’s disease is not usually apparent until more than 90% of the adrenal cortex has been destroyed, so that very little adrenal capacity is left.
This can take months to years and is known as primary adrenal insufficiency.
Addison’s disease signs and symptoms, once advanced, include:
- Severe fatigue, weakness
- Weight loss
- Dizziness
- Increased need for salt
- Increased skin pigmentation
- Feeling faint
- Low blood pressure
- Nausea
- Vomiting
- Painful muscles and joints
- Hair loss
If Addison’s disease is left untreated, it eventually leads to an adrenal crisis, which is a medical emergency. This is where the symptoms of Addison’s disease appear quickly and severely.
How is it diagnosed?
In its early stages, Addison's disease can be difficult to diagnose. A typical Addison's disease diagnosis includes your doctor reviewing your early symptoms, asking you about your family history and giving you a physical examination. Symptoms, especially the darkening of the skin, may lead a doctor to suspect Addison's disease.
This will be followed by laboratory tests, which aim to determine cortisol levels, and to then establish the cause. Imaging of the adrenal and pituitary glands are also used.
Other tests include:
- Blood test
- Urine test
- Synacthen stimulation test
- A thyroid function test
- Scans, either computerised tomography (CT) scan or a magnetic resonance imaging (MRI) scan
What are your treatment options?
Treatment is aimed at replacing lost hormones. You will need lifelong treatment with steroid replacement therapy. With the right balance of daily medication, the prognosis for a healthy life is good and most people with the disease are able to continue life much as it was before their illness.
Cortisol is replaced orally with tablets containing a synthetic glucocorticoid, taken once or twice a day.
If aldosterone is also deficient, it’s replaced with oral doses of a mineralocorticoid.
Medications for Addison’s disease don’t typically have side effects as they merely replace the lost hormones. If you take a higher dose than necessary for a long time, however, there's a risk of problems such as osteoporosis, mood swings and insomnia.
You and a partner or family member may be trained to administer an injection of hydrocortisone in an emergency, that is, an Addison’s crisis.
This could be necessary if you go into shock after an injury, or if you experience vomiting or diarrhoea and are unable to keep down oral medication. This may occur during pregnancy with morning sickness.
Can it be prevented?
It isn’t possible to prevent Addison's disease, but you can focus on relieving symptoms and preventing Addison's-related medical emergencies.
Prevention may include treating underlying conditions and limiting risk factors.
These factors may help prevent Addison’s disease:
- Treating fungal infections
- Controlling diabetes
- Identify cancer symptoms to prevent spread of cells into adrenal glands and bloodstream
- Treating bacterial infection such as tuberculosis (TB)
