A rare but potentially life-threatening disorder, an epidural abscess is a collection of pus situated between the skull bones and the brain lining, or between the bones of the spine and the outer membrane of the spinal cord.
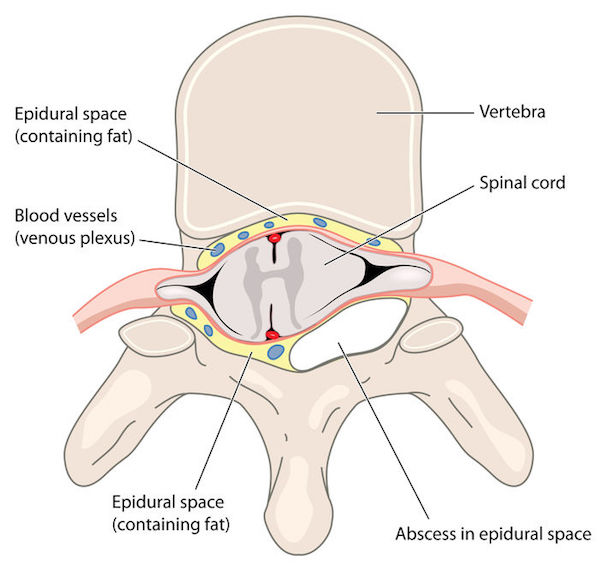
This pus infection causes inflammation, pressing up against the bones and the meninges, that is, the membranes that protect the spinal cord and the brain. It can adversely impact physical movement and sensations. If it is not treated correctly, permanent nervous system damage or death can occur.
Epidural abscess can present in the skull – known as an intracranial epidural abscess (IEA) – or in the spine area, known as a spinal epidural abscess (SEA).
It is usually caused by a bacterial infection such as Staphylococcus aureus, but it could also be due to infection by a fungus or another germ. Often though, doctors struggle to identify a specific cause.
However, the causes of an IEA could include:
- Chronic ear infections such as otitis media (inflammation of the middle ear)
- Craniotomy (the surgical removal of part of the bone from the skull to expose the brain)
- Head injury
- Mastoiditis (an infection of the mastoid bone of the skull, normally caused by a middle ear infection)
- Neurosurgery
- Sinusitis
Those who have the following conditions may be at risk of a SEA:
- Alcoholism
- Bloodstream infections
- Boils, specifically on the back or scalp
- Bone infections of the spine (vertebral osteomyelitis)
- Diabetes mellitus
- Intravenous (IV) drug use
- Recent back surgery or other spinal operations
- Renal (kidney) insufficiency
Most studies indicate that epidural abscess is more common in men than in women.
What are its symptoms?
An epidural abscess is a medical emergency, so go straight to your doctor or the emergency room at a hospital if you notice the symptoms below. An early diagnosis and speedy treatment are vital to ensure that serious complications don’t occur.
The symptoms of an intracranial epidural abscess (IEA) may include:
- Fever
- Headache
- Lethargy
- Loss of sensation such as numbness in any area of the body, or abnormal changes in sensation
- Nausea and vomiting
- Problems with coordination and movement
- Weakness
The symptoms of a spinal epidural abscess (SEA) may include:
- Fever
- Back pain
- Difficulty urinating
- Inability controlling bowel or bladder
If not treated, serious complications can include the following:
- Abscess in the brain or of the spinal cord itself
- Bone infection (osteomyelitis)
- Brain damage
- Infection inside the spine or skull
- Irreversible damage to the brain or nervous system, such as paralysis
- Long-term chronic back pain
- Meningitis
- Nerve damage
How is it diagnosed?
A doctor may make use of several tests to make a diagnosis. They may include:
- Blood cultures
- A complete blood count (CBC)
- MRI (magnetic resonance imaging) scan of head or spine
- CT (computerised tomography) scan of head or spine
- Draining of the abscess so that a sample of fluid from the infected area can be examined.
What are your treatment options?
As it affects your brain or spine directly, an epidural abscess is a serious health issue. The sooner it is treated, the better your chances of not having to deal with the damaging effects of complications.
Antibiotics are generally the course of treatment prescribed for at least four to six weeks. Some patients may need to take antibiotics for a longer duration, depending on how aggressive the infection is.
A surgeon may need to drain the fluid from the abscess with a needle to alleviate the build-up in pressure, or they may need to remove it entirely. Surgery will occur when movement is difficult, or there is a loss of sensation such as numbness, or paralysis.
Can it be prevented?
Ensure you get treated promptly for any infection, particularly blood infections, sinus or ear infections to prevent the development of an epidural abscess.
IMAGE CREDIT: 123rf.com
