A rare medical condition, infective endocarditis (IE) occurs when harmful bacteria enter your bloodstream and infect the inner lining of your heart (endocardium), a heart valve or a blood vessel.
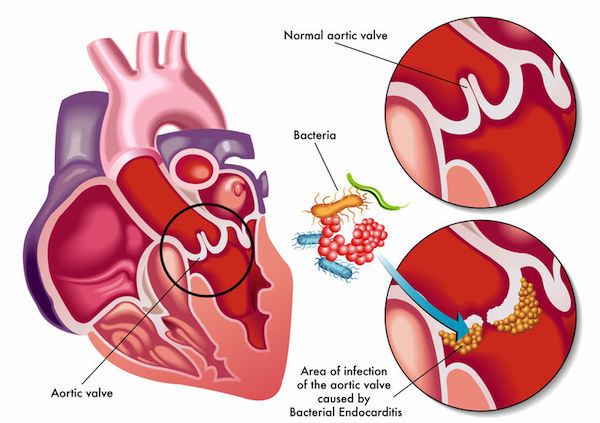
IE sees bacteria from, for example, your mouth, spreading throughout your bloodstream and affixing to damaged areas in the heart, including damaged heart tissue or abnormal heart valves.
An uncommon medical condition, it is more prevalent in developing countries than it is in the Western world.
Bacteria – such as Streptococcus viridans and Staphylococcus aureus – most commonly cause IE, although fungi and other microorganisms may be responsible. The culprit may enter your bloodstream through a myriad ways, including:
- An infection or medical condition: This could include a skin sore, gum disease, a sexually transmitted infection (STI) or an intestinal disorder such as inflammatory bowel disease (IBD).
- Catheters or needles: The harmful bacteria may be introduced into your bloodstream by a catheter, which is a thin tube used by medical practitioners to inject or remove fluid from your body. Any contaminated needle or syringes, for example, those used for illegal drug use or even tattooing could also allow the bacteria in.
- Daily oral activities: Brushing your teeth, picking your teeth with a toothpick or just chewing food could allow harmful bacteria to enter your bloodstream, particularly if you have unhealthy teeth and gums.
- Dental procedures: Some dental procedures that cut open your gums may allow bacteria in.
If it isn’t treated, it can damage and destroy your heart valves and lead to life-threatening complications, including stroke and organ damage, abscesses in the heart, brain, kidneys, spleen and liver, and heart failure.
People with healthy hearts are unlikely to be infected by IE. However, those with underlying heart conditions have the highest risk of developing it, including those with:
- Post-rheumatic fever damaged heart valves
- An abnormality of the heart valves after a heart transplant
- Artificial heart valves or heart valves repaired with artificial materials
- A history of endocarditis
- Damaged heart valves
- Some types of congenital heart defects
Illegal drug users who inject their drugs are also at a greater risk.
What are its symptoms?
Endocarditis can develop rapidly or slowly, depending on the cause of the infection and if you suffer from a heart condition. Signs and symptoms could include:
- Aching joints and muscles
- A new or changed heart murmur
- Blood in your urine
- Fatigue
- Fever and chills, including night sweats
- Delirium
- Janeway lesions, which are painless, often haemorrhagic (bleeding into the skin) lesions that occur on your palms and soles
- Persistent cough
- Red, tender spots under the skin of your fingers (Osler’s nodes)
- Swelling in your feet, legs or abdomen
- Shortness of breath
- Tiny purple or red spots on your skin, inside your mouth or in the whites of your eyes (Petechiae)
- Unexplained weight loss
If you develop these signs and symptoms see your doctor immediately.
How is it diagnosed?
Your doctor will do a physical examination checking signs and symptoms, and speak to you about your medical history, particularly any heart disorders you may have. You may then be referred to a cardiologist.
Your doctor may make use of several tests to make a diagnosis, including:
- Blood tests: These will identify any offending bacteria, as well as any medical conditions, such as anaemia that may be an indication of IE.
- Chest X-ray: This will show whether endocarditis has enlarged your heart or if the infection has impacted your lungs.
- CT (computerised tomography) or MRI (magnetic resonance imaging) scans: These will show where the infection has spread to in your body.
- Transesophageal echocardiogram: This will allow your doctor to get a close view of your heart valves by inserting an ultrasound device into your mouth and oesophagus.
- Urine test for blood, protein or casts
What are your treatment options?
Endocarditis treatment includes antibiotics for two to six weeks. This could entail high doses of intravenous (IV) antibiotics administered in hospital initially.
You may need surgery if your heart valves have been severely damaged, or if the IE was caused by a fungus. Surgery could entail repairing a damaged valve or replacing it with an artificial one.
It is reported that patients with IE have a 70% survival rate with effective treatment. The most common cause of death for IE patients is intractable heart failure.
Can it be prevented?
Practicing good hygiene is a necessity when it comes to helping prevent endocarditis. This includes:
- Taking good care of your dental health, including brushing and flossing regularly, and having regular check-ups.
- Avoiding procedures that could possibly lead to skin infections, including tattooing and piercings.
- Ensuring you get prompt medical assistance if you develop any skin infections or open sores.
To prevent IE, those who suffer from the following conditions may need to take preventative antibiotics before specific medical or dental procedures:
- Rheumatic heart disease
- An abnormality of the heart valves after a heart transplant
- Artificial heart valves or heart valves repaired with artificial materials
- A history of endocarditis
- Certain types of congenital heart defects
IMAGE CREDIT: 123rf.com
